How EHR Integration Improves Healthcare Practice?
Electronic health records have become integral to the system in the fast-evolving healthcare sector. EHR integration allows different healthcare systems to communicate. Such as hospitals, clinics, and laboratories. To share and access patient information securely in real-time. This eliminates paperwork, reduces errors, and enhances communication between healthcare professionals.
Despite the numerous benefits of EHR. Many healthcare organizations are unaware of the potential of EHR and how it has revolutionized the healthcare system. In this guide, we have covered everything about EHR integration, its benefits, challenges in EHR integration, and best practices to utilize it efficiently.
Table of Contents
- What is EHR Integration?
- Types of EHR Integration
- What Problems Does EHR Integration Solve?
- Benefits of EHR Integration
- Step-By-Step Process For EHR Implementation
- Common EHR Integration Challenges and Solutions
- Best Practices For EHR Integration in Healthcare
- Top EHR Integration Tools
- Future Trends in EHR Integration
- Conclusion
- FAQs
What is EHR Integration?
EHR integration is a process of connecting different healthcare systems. This allows healthcare providers to access, share, and update patient records in real time, regardless of where the patient received treatment. It ensures patient data is easily accessible and efficiently managed across different healthcare touchpoints. Previously, patient information was stored on physical paper. They did not communicate with each other. This creates challenges, such as missing medical history, duplicate tests, and delays in treatment. EHR integration software solves these problems. By ensuring all patient data is available virtually in one connected system.
Types of EHR Integration
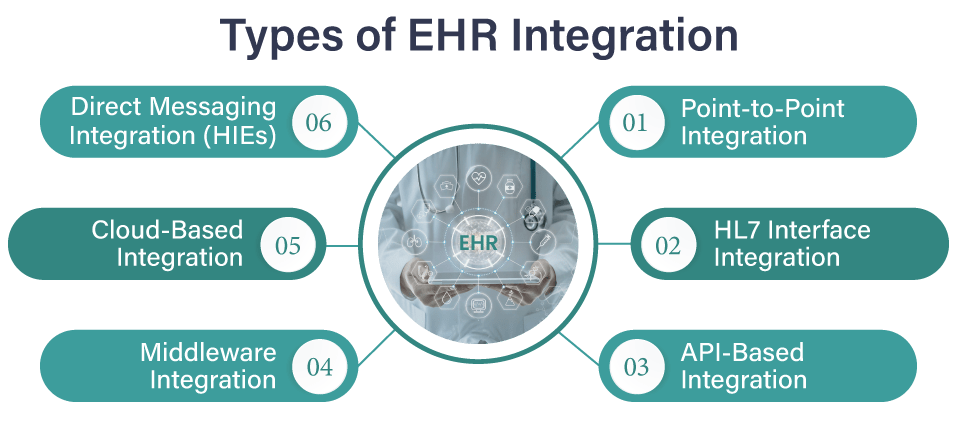
Here are some popular types:
1. Point-to-Point Integration
Point-to-point integration is simply making a direct link between two healthcare systems. So that patient information can be exchanged. It is a simple and inexpensive solution for small healthcare businesses that do not have a lot of systems to integrate, like EHR and scheduling appointments. The larger your business becomes and adds systems, the more difficult this method is to deal with, since each new system needs its own connection.
Best For: Small to mid-sized healthcare organizations with fewer systems requiring integration.
2. HL7 Interface Integration
HL7 is a worldwide standard for the exchange of healthcare data. By using HL7 interfaces, different systems, such as hospitals, laboratories, and pharmacies, can share patient information in a standard format easily. It minimizes errors, makes data easy to interpret, and enhances provider coordination. It is perfect for high-volume data-sending practices.
Best For: Healthcare providers looking to standardize data exchange across multiple platforms.
3. API-Based Integration
APIs (Application Programming Interfaces) act like messengers, allowing different software systems to communicate with one another. If your practice needs to connect several applications like EHRs, scheduling tools, and telemedicine systems. It has great scalability and flexibility. As your business grows, the system can expand with changing needs.
Best For: Healthcare organizations need agile and scalable solutions for integrating multiple applications.
4. Middleware Integration
Middleware is a link that connects various systems within a company. Rather than each system being directly connected to the other systems, middleware makes it easier for all the systems to be connected to one platform. It is ideal for large companies that have a great number of various systems being utilized, as it makes things easier to communicate and easier to handle.
Best For: Large healthcare organizations with multiple systems require seamless communication.
5. Cloud-Based Integration
Cloud-based integration stores patient data securely in the cloud, where it is accessible anywhere. This saves the cost of on-site servers and offers secure, remote access. It is a valuable feature, particularly in the aftermath of the growth of telemedicine.
Best For: Healthcare organizations looking for scalable and cost-effective integration solutions.
6. Direct Messaging Integration (HIEs)
Direct messaging interoperability, usually used in Health Information Exchanges (HIEs), enables healthcare professionals to safely send and receive patient information between systems. It is especially vital in care transfers, for instance, when the patient is being transferred from one physician to another. Direct messaging will give all the involved parties up-to-date information, improving communication, reducing medical mistakes, and allowing for improved care of the patients.
Best For: Providers seeking to improve care transitions and secure communication.
What Problems Does EHR Integration Solve?
Here are some key problems EHR integration solves:
1. Fragmented Patient Data
Problem: Patient information is shared in different systems, and it is hard for doctors to get the whole, up-to-date picture of the patient’s condition in one place. This can lead to decisions being made on incomplete or outdated information.
Solution: EHR integration puts all systems on one platform and builds one record for the patient. This reduces errors and gives doctors up-to-date information, improving decision-making and treatment.
2. Data Sharing and Interoperability
Problem: Health systems do not communicate well. It leads to delays and inaccuracies in sharing patient information between hospitals, clinics, and labs.
Solution: Integration of EHR standardizes data exchange. It enables secure, continuous sharing of information between systems. This improves care coordination, accelerating treatment and making it more precise.
3. Inefficient Communication
Problem: Slow communication, relying on outdated methods like phone calls or faxes, increases the risk of miscommunication and medical errors.
Solution: EHR integration provides real-time access to patient data, improving communication between doctors, nurses, and specialists, leading to quicker, more coordinated care.
4. Limited Access to Patient Information
Problem: Patient data stored in paper files or scattered systems can be difficult to access, especially in emergencies, delaying care.
Solution: EHR integration stores data electronically and ensures it’s accessible from anywhere, speeding up care and improving decision-making, especially in urgent situations.
5. Billing and Coding Errors
Problem: Manual billing and coding are prone to mistakes, causing delays in payments or errors in insurance claims.
Solution: EHR integration automates billing and coding, reducing errors, speeding up payments, and ensuring accurate reimbursements.
Read Also: Ultimate Guide To Master 99214 CPT Code in 2025
6. Compliance and Regulatory Challenges
Problem: Healthcare organizations must manage strict regulations like HIPAA, which can be complex and time-consuming.
Solution: EHR integration helps maintain compliance by securely storing and transmitting data, ensuring only authorized access and keeping records of usage, reducing risk, and protecting patient privacy.
📲 Curious About How EHR Integration Can Benefit Your Practice?
💬 Chat with Our Experts on WhatsApp
Let’s TalkBenefits of EHR Integration
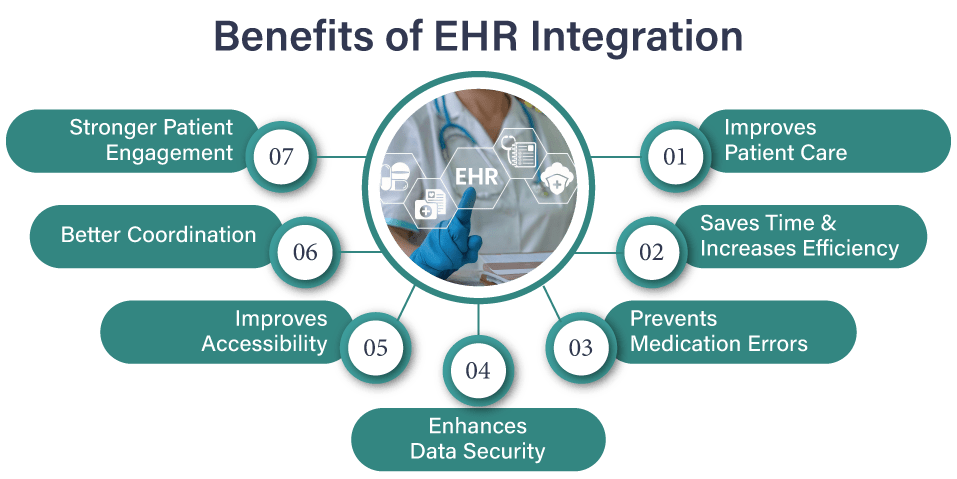
Here are some significant benefits of EHR integration:
1. Improves Patient Care
With EHR, doctors can see your complete medical history in one place, which includes past treatments, allergies, and test results. This helps them make faster and better decisions about your health. EHRs also alert doctors to possible medication issues. It keeps you safer.
2. Saves Time and Increases Efficiency
EHRs reduce paperwork and make things faster. Doctors and nurses do not have to spend time searching for files or writing down the same information repeatedly. Scheduling, billing, and record-keeping happen automatically. So medical staff can focus on patient care.
3. Prevents Medication Errors
EHRs check your medications to make sure they do not cause harmful reactions, especially with other drugs you are taking. If there is a problem, doctors get an alert right away. This helps prevent dangerous mistakes and keeps you safe.
4. Enhances Data Security
Paper records can be lost, stolen, or damaged. EHRs store your health data securely with passwords and encryption. So only the right people can access it. Plus, regular backups prevent accidental data loss.
5. Improves Accessibility
Doctors can quickly pull up your medical history remotely from anywhere. Whether in a hospital, clinic, or even during an emergency. You can also check your health records online. So you always know what is going on with your care.
6. Better Coordination
When you see different doctors or specialists. EMR vs EHR helps them share your information quickly. This way, everyone involved in your care stays updated and avoids confusion. It ensures you get the best treatment.
7. Stronger Patient Engagement
EHRs let you see your medical records, test results, and appointments online. You can securely message your doctor, ask questions, and request prescription refills without visiting the clinic. This makes it easier to manage your health.
Step-By-Step Process For EHR Implementation
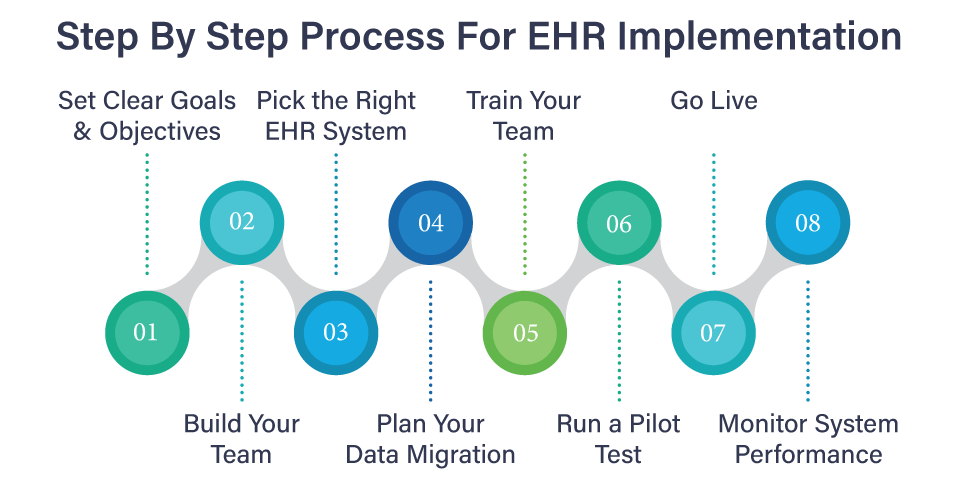
Here are the simple steps for the EHR implementation process:
1. Set Clear Goals & Objectives
Start by deciding what you want to achieve with your EHR system. If you want to enhance patient care, accelerate billing, or reduce errors, knowing what you wish to accomplish will direct your entire project. Be certain that you and all who are working for you know what you are after.
2. Build Your Team
You need the right staff for a successful EHR software implementation. This includes a project manager to oversee all the operations and IT staff to perform technical tasks. Plus, healthcare staff like doctors and nurses help with everyday needs. You need the right team with the right combination of skills.
3. Pick the Right EHR System
Choose an EHR system that is most appropriate for your practice. Determine what you need in terms of features, such as scheduling or telemedicine. Then, find out whether the system is compatible with other software that you are using. Do not be in a rush to research and choose that which is most appropriate for you.
4. Plan Your Data Migration
Patient data transfer to the new system is a big project. Make sure you plan so that you don’t end up losing any important information. Classify the information, check it for errors, and then transfer it to the new system in phases. That way, you won’t get any confusion later on.
5. Train Your Team
Now, it is time to train the staff. Everyone will be utilizing the system, from the physicians to the administrative staff. They need to know how the system works. Provide them with hands-on training. So they can get familiar with the system and be able to assist as and when needed.
6. Run a Pilot Test
Before you fully switch to the new system, test it with some of the users. The test will catch any faults and fix them before putting all the users on the system. Take feedback and adjust to make the experience smoother.
7. Go Live
After testing, you can then go live with the EHR system for all patient data. There will be some glitches initially, but with good planning and training, this will be a seamless transition.
8. Monitor System Performance
Once the system is live, track how it is doing. In case there are problems, solve them on time. Also, track whether the system is helping you in your intent, whether it is reducing errors or streamlining processes, and adjust accordingly.
Common EHR Integration Challenges and Solutions
Here are some significant challenges when integrating the EHR system:
1. System Compatibility Issues
Healthcare facilities use different software for billing, scheduling, and patient records. Suppose the new EHR does not work well with these systems. It can create problems.
Solution: Choose an EHR that quickly connects with other tools. It can help avoid this issue.
2. High Costs
EHR systems are expensive. Organizations must decide whether to build their system or buy one from a vendor. Each option requires money, time, and resources.
Solution: Careful planning is necessary before making a choice.
3. Staff Training and Adoption
Not all staff members are comfortable using a new system. Some might find it confusing or frustrating.
Solution: Proper training and support are needed to help them learn and adjust smoothly.
4. EHR Data Migration Issues
Moving patient records from the old system to the new one can be tricky if data is lost, incorrect, or formatted differently. It can cause delays and errors.
Solution: Working with a trusted vendor ensures safe and accurate data transfer.
5. Data Privacy Concerns
Protecting patient information is critical. This is especially true with rising cybersecurity threats.
Solution: The EHR system must have strong security features. Such as encryption and strict access controls. To prevent data leaks or breaches.
6. Measuring Return on Investment
EHR systems take time and money to set up. So, organizations want to see clear benefits, such as improved efficiency and better patient care.
Solution: Tracking performance and workflow improvements can help determine if the investment was worthwhile.
Looking for a White-Label Telemedicine Platform?
Launch a branded telemedicine solution that reflects your practice’s identity.
Contact Us NowBest Practices For EHR Integration in Healthcare
Here are some best practices to follow for successful EHR integration:
1. Planning
First, you should start with an in-depth analysis of your existing system and workflows to clearly define your goals and objectives for the EHR integration.
2. Pick the Right EHR System
Choose an EHR that quickly connects with other healthcare systems. To simplify data sharing. You should look for one that follows industry standards. Such as FHIR and HL7. A good EHR interoperability will work well with telehealth platforms and remote patient monitoring tools.
3. Choose a Trustworthy Vendor
Your EHR provider should offer firm support and reliable service. Research different vendors and read customer reviews. And check if other organizations have had success with them. Ensure they provide training, tech support, and regular updates. To keep the system running smoothly.
4. Involve Your Team Early
Doctors, nurses, and administrators should be part of the process. Clearly define their roles and responsibilities. So everyone knows what to do. Getting input from all stakeholders. It ensures the system meets everyone’s needs.
5. Listen to Patient Feedback
Patients should also have a say in how the EHR system integrates. You should conduct surveys or hold discussions to understand the patient’s concerns and preferences. Use their feedback to make the system easier to schedule, access, and communicate with doctors.
6. Train Your Staff Properly
Not everyone will be familiar with the new system. So, proper training is essential. Offer training sessions tailored to different job roles. Use a mix of in-person workshops, online courses, and hands-on practice, which makes learning easier.
7. Keep Learning and Improving
Technology keeps changing. So, ongoing training is essential. Schedule refresher courses to help staff stay updated on new features. Encourage employees to share tips and best practices for continuous improvement.
Top EHR Integration Tools
Here are the five best EHR-integrated software:
1. NexHealth
A patient-friendly platform. It connects with different EHR systems using its fast integration tool. It helps with online scheduling, patient communication, and digital paperwork, saving your practice time.
2. eClinicalWorks
A complete healthcare tool. It includes EHR, telehealth, and billing management. It also has a virtual assistant, “Eva,” who helps doctors analyze patient data and improve diagnoses.
3. CareCloud
A full-featured system that manages patient flow, prescriptions, and billing. It also provides real-time insights, which help doctors make better treatment decisions.
4. Athenahealth
A simple cloud-based EHR system integration. It works on multiple devices. It is excellent for small and medium-sized clinics that want an easy system without technical expertise.
5. TheraNest
An excellent tool for mental health professionals. It offers digital patient records, therapy notes, and billing support. It also helps practices handle insurance claims more efficiently.
Looking for a reliable telemedicine app solution?
Connect with industry-leading developers in the USA.
Get a free consultation today ↗Future Trends in EHR Integration
Explore some future trends in EHR integration:
1. Increased Adoption of FHIR Standards
Overview:
FHIR (Fast Healthcare Interoperability Resources) is becoming the new standard for healthcare data sharing. It allows different healthcare systems to communicate and exchange information smoothly.
Why it matters:
- FHIR allows for real-time data exchange between systems.
- It simplifies the integration process by offering a standardized format.
- It helps reduce data silos, improving care coordination.
Future Impact:
As FHIR is adopted more widely, healthcare systems will exchange information instantly and accurately, which makes it easier for doctors to coordinate care. This will result in faster, more efficient treatment with fewer errors.
2. Artificial Intelligence and Machine Learning
Overview:
AI and machine learning are technologies that are being integrated into EHR systems. It helps to assist with data analysis and decision-making, which makes healthcare smarter and more efficient.
Why it matters:
- AI can automate repetitive administrative tasks, saving time.
- Machine learning can provide predictive insights to assist in diagnosis and treatment.
- It can help reduce human errors and improve patient outcomes.
Future impact:
AI and machine learning will enable early disease detection and personalized treatment. They help healthcare providers make quicker, more accurate decisions. This will ultimately improve the overall quality of care. Plus, they allow healthcare workers to focus more on patients.
3. Data Security and Privacy Enhancements
Overview:
As healthcare data moves online, stronger security measures like encryption and blockchain will be implemented. It protects sensitive patient information from cyber threats.
Why it matters:
- Stronger security measures protect sensitive patient information from breaches.
- Ensures compliance with regulations such as HIPAA.
- Builds trust with patients, ensuring their data is protected from unauthorized access.
Future impact:
Stronger security measures will protect patient data from breaches. It builds trust in digital healthcare systems and ensures compliance with privacy regulations.
4. IoT and Wearable Device Integration
Overview:
Devices like smartwatches, fitness trackers, and other IoT devices collect real-time health data, such as heart rate or activity levels. It can be shared directly with healthcare providers via EHR systems.
Why it matters:
- These devices provide continuous, real-time monitoring of patient health.
- Doctors can track patients’ progress and intervene if there’s a problem, even if the patient isn’t at the clinic.
- It allows for better management of chronic conditions, reducing hospital visits.
Future impact:
IoT devices and wearables will allow doctors to manage patients’ health more proactively by tracking real-time data. This will help catch health issues earlier and reduce hospital visits, improving patient outcomes and overall care convenience.
5. Cloud-Based EHR Systems
Overview:
Cloud-based EHR systems store patient data securely online, which makes it accessible from anywhere and reduces the need for on-site IT infrastructure.
Why it matters:
- Cloud systems are more flexible, allowing doctors to access patient data from anywhere.
- They are cost-effective and reduce the need for expensive IT infrastructure.
- Updates to the system can be done quickly and automatically, ensuring the system is always up-to-date.
Future impact:
More healthcare practices will use cloud-based EHRs. It makes patient records easier to access. It will improve collaboration between providers, even across regions. Cloud tech will also make EHRs more secure and scalable as practices grow.
6. Telemedicine Integration
Overview:
Telemedicine has grown in popularity, especially since the COVID-19 pandemic. By integrating telemedicine with EHR systems, doctors can access patient records during virtual consultations.
Why it matters:
- Telemedicine integration provides a full view of a patient’s health, even during remote visits.
- It increases access to healthcare, especially for patients in rural or underserved areas.
- It ensures continuity of care, as virtual visits are recorded in the same EHR system as in-person visits.
Future impact:
Telemedicine will become a standard part of healthcare, allowing more people to access care from anywhere. Integration with EHR systems will improve the efficiency and accuracy of virtual visits, which makes healthcare more accessible and convenient.
Conclusion
EHR integration enhances healthcare by streamlining patient data management, reducing paperwork, and preventing medical errors. Despite its benefits, many healthcare organizations have not yet utilized its potential. We hope this guide helps you understand the role of EHR in the healthcare system, its benefits of EHR integration, the roadmap to implement EHR, and the best practices to follow. However, many healthcare organizations are not technically proficient, and at this point, hiring an experienced development firm can be a great idea. So you can let the professionals integrate EHR into your systems.
So, if you are planning to integrate EHR into your healthcare system, VCDoctor is a one-stop telemedicine app development company. We specialize in customizing to match your unique business identity and enhance patient care.
FAQs
Q1. What is the difference between EMR vs. EHR integration?
EMRs store patient data for a single healthcare provider. While EHRs share patient records across multiple providers.
Q2. How does EHR integration improve patient care?
It streamlines data sharing, reduces medical errors, and improves diagnosis accuracy. It enhances treatment efficiency.
Q3. What are the costs associated with EHR integration?
Costs depend on system complexity, customization, and ongoing maintenance.
Q4. What is the role of HL7 standards in EHR integration?
HL7 provides standardized protocols for seamless data exchange between different healthcare systems.
Q5. How can I measure the ROI of EHR integration?
ROI can be measured through improved workflow efficiency, cost savings, reduced errors, and better patient outcomes.
Q6. What are the everyday challenges of EHR integration?
Challenges include high costs, data security concerns, interoperability issues, staff resistance, and regulatory compliance.




