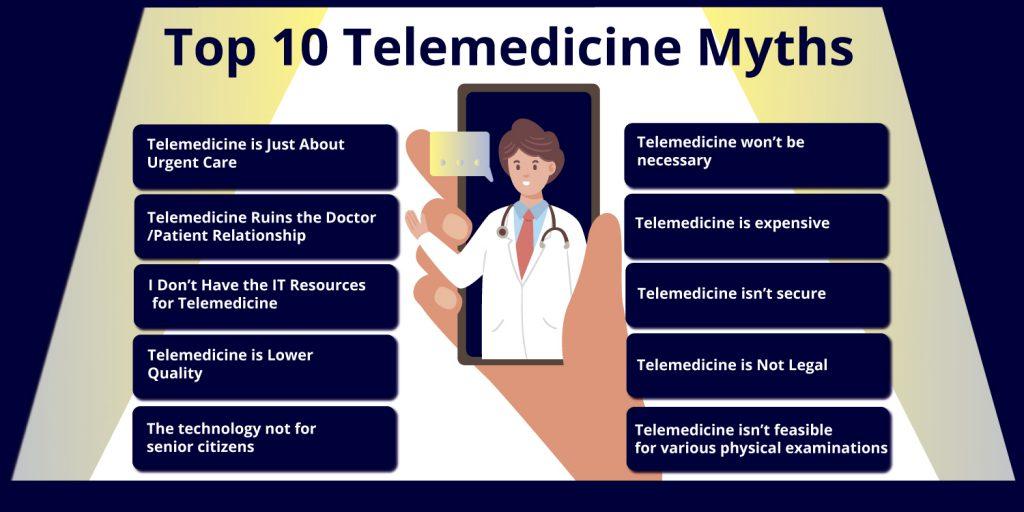
Debunking Top 10 Telemedicine Myths
In the world of advanced technologies, it’s common to have some myths about a particular technology. Telemedicine is no different; the healthcare market is brimming with these telemedicine myths. You will be surprised to know that people on the Internet are attracted to more negative things than positive ones. In this blog, we will be debunking several top myths of Telemedicine that are prevailing in the global market.
Given the particularly slow adoption of technology in healthcare, the idea of telemedicine might still be new to clinicians and physicians. Telemedicine is gaining ground. Telemedicine platforms is described simply as “the remote distribution of healthcare services.” Myths About Telemedicine topic is very popular in this time.
Many people misunderstand that telemedicine isn’t legal and pricey, much more. Telemedicine software Development Company is at a rising and growing stage but people still feel insecure and have misconceptions that make people refuse to embrace telemedicine. But first, let’s get an overview of Telemedicine.
Telemedicine: An Overview
Many people wonder what Telemedicine myths really mean and how it works. The term “telemedicine” refers to a system in which medical advice and treatment are provided to patients at a distance. Tele means “far away” and is a Greek word.
This can be a simple scenario where two or more medical experts discuss a specific case over the phone, or it can be as complex as two surgeons discussing the operation through a teleconferencing system while the operation is actually taking place in the operating room.
The distance between professionals is not limited as long as they are connected via a computer network and can be located at two points on the globe. Telemedicine services may also involve the use of unmanned robots that transmit medical files and information to healthcare professionals over a network anywhere.
Telemedicine is the use of communication technology to access and provide medical care to patients. Many hospitals and institutions also call this “remote care.” This is nothing new in the medical world.
In this article, we will debunk some of the Telemedicine myths.
Top 10 Telemedicine Myths
Myth 1: Telemedicine is Just About Urgent Care:-
Although true telemedicine systems may be a nice option for attending an emergency room or the ER, this is not the only advantage. 60 percent of those polled say they want to see a specialist online to better treat their health illnesses. This makes a lot of sense because patients with chronic illnesses usually know exactly what’s going on and how they can address their needs face-to-face with a specialist over the phone.
Myth 2: Biggest Telemedicine Myths that Ruins the Doctor/Patient Relationship:-
Telemedicine is not supposed to be a replacement for face-to-face appointments at a doctor’s office. Rather, it is intended to act as a complement to appointments by regular physicians. Telemedicine myths are perfect for occasions where you are unable to make an appointment with your primary care specialist and the condition is not serious enough for an emergency room ride. Telemedicine is a reasonable choice in many non-emergency cases where medical treatment can be provided without a doctor’s or online doctor’s visit.
Myth 3: I Don’t Have the IT Resources for Telemedicine:-
You then have all the required IT tools. Video chat applications were developed with the goal to be easy to use, removing the need to download specific apps or something new. You can keep a virtual meeting if you can make a phone call.
The more you invest in a Telemedicine service provider, the more services you can provide patients with.
In the case of telemedicine services, it’s just not the case of the adage “you get what you pay for.” More expensive telemedicine portals include virtual waiting rooms, a segment of the telemedicine application to record visits, patient options to pay for treatments, screen sharing, and more. These copy many of the functions on benefits of EHR and your patient site. In my experience, you want to interact effectively and easily with patients from both the provider’s and the patient’s viewpoint.
Myth 4: Telemedicine is Lower Quality:-
Not every patient can be treated remotely or those patients should be sent to a physical place. It is critical for all patients who do undergo virtual treatment that clinicians meet the same quality criteria as their counterparts in conventional hospitals, including integrating case analysis as part of the quality management process.
Our research indicates that 64 percent of people needing treatment in a virtual pharmacy will be treated online. The remaining 36 percent are given medically appropriate referrals to the conventional hospitals of the health system.
Another way to measure quality is by analyzing prescribing rates. The rate of medication for those seeking telemedicine is comparable with people attending conventional clinics?
Myth 5: One of the biggest telemedicine myths is that it’s Not Legal:-
As new technology arises, new laws and policies do so, but not at the same time; thus it is understandable that many people believe that Telemedicine is not legal. Rest assured, telehealth is perfectly legal as long as there are appropriate protections in effect, all of which are governed under the Health Insurance Portability and Accountability Act (HIPAA). You need to guarantee, for example, that you use safe, HIPAA-compliant video conferencing.
Myth 6: Telemedicine is expensive
The answer to the question that asks about the affordability of telehealth services varies a lot, depending on an individual’s income, access to care, covered workers’ benefits, and geographical location. However, there are aspects of Telemedicine that are very cost effective and can make sense for you and your specific situations.
According to a recent study, telehealth services reduced the length of time in the intensive care unit by thirty percent, which significantly reduced health care costs. In the case of chronic health problems, distance health reduces costs by providing patients with the care and treatment plans they need from the outset.
Join the telemedicine revolution and take advantage of this innovative Telemedicine Platform today!
Myth 7: Once the pandemic is over, Telemedicine won’t be necessary
Fear of the coronavirus has prompted patients to meet with their doctors, pediatricians, therapists, and counselors via computers, mobile phones, and virtual reality. During the pandemic, Telemedicine has helped healthcare professionals differentiate some patients through virtual consultation using new technologies. To protect patient privacy.
Examining patients before going to a clinic or ambulance increases efficiency and safety, as patients who have previously been treated usually spend less time waiting for treatment, and providers have a much more derivative understanding of what services are needed. Telemedicine can also provide timely guidance to patients at risk. Telehealth benefits for patients are huge, and patients love it. The branch of Telemedicine is here to stay.
Myth 8: Telemedicine isn’t secure
Let’s debunk another Telemedicine myth with recent statistics; the telemedicine services market is growing rapidly, which means that the amount of personal data transmitted through telemedicine solutions is also growing. Thus, the issue of telemedicine security is becoming increasingly important, as leakage of PHI (Protected Health Information) causes serious financial and reputational damage to telemedicine service providers.
Myth 9: The technology not for senior citizens
Telemedicine in the health sector uses a web application or a telephone call to help doctors and patients connect remotely. Through these visits, patients can manage conditions such as diabetes, respiratory infections, and even depression without even satisfying the condition to physically go to the office or clinic.
Although Telemedicine has gained popularity over the past decade, Telemedicine now offers a special advantage to patients of all ages, but especially to older adults: safety from exposure to COVID-19. This refutes another telemedicine myth that it is not viable for the elderly.
It can provide a convenient way for older people to manage their health. In the middle of a COVID-19 pandemic, a virtual visit with a service provider can help limit their exposure to the virus. However, it can be difficult to adapt to the necessary technology and address the physical disabilities that can hinder access to healthcare through Telemedicine.
Myth 10: This also a Telemedicine Myths that isn’t feasible for various physical examinations
Telemedicine has attracted a lot of telemedicine myths about its way of operation. One of which is; it’s not feasible for practical examination. Let’s head to the answer. Most people are probably thinking about real-time Telemedicine for the first time when they hear the word “telemedicine.”
Real-time Telemedicine requires live communication, either between a healthcare professional and a patient or between healthcare professionals using audio and video communications. Think video chat. However, there are several real-time telemedicine software that is much more comprehensive than a simple video chat software or an app, the primary goal is to see and talk to the patient from afar. This type of Telemedicine is designed to provide a virtual alternative to a personal doctor’s visit.
Physicians are also beginning to adopt real-time telemedicine solutions to provide their patients with additional convenience for virtual doctor visits, improved treatment outcomes, improved work-life balance, and many other telehealth benefits. Easily compatible with your device, internet connection, microphone, and webcam; every patient now receives medical care. We hope that clears your mind about this myth.
The Final Takeaway for Telemedicine Myths!
There are a number of reasons to be optimistic about the future of Telemedicine. With the speedy development in the field of healthcare technology, Telemedicine is likely to become simpler and more widely accepted in the coming years. Already smart glasses can monitor patients’ health data and transmit it to healthcare professionals in real-time.
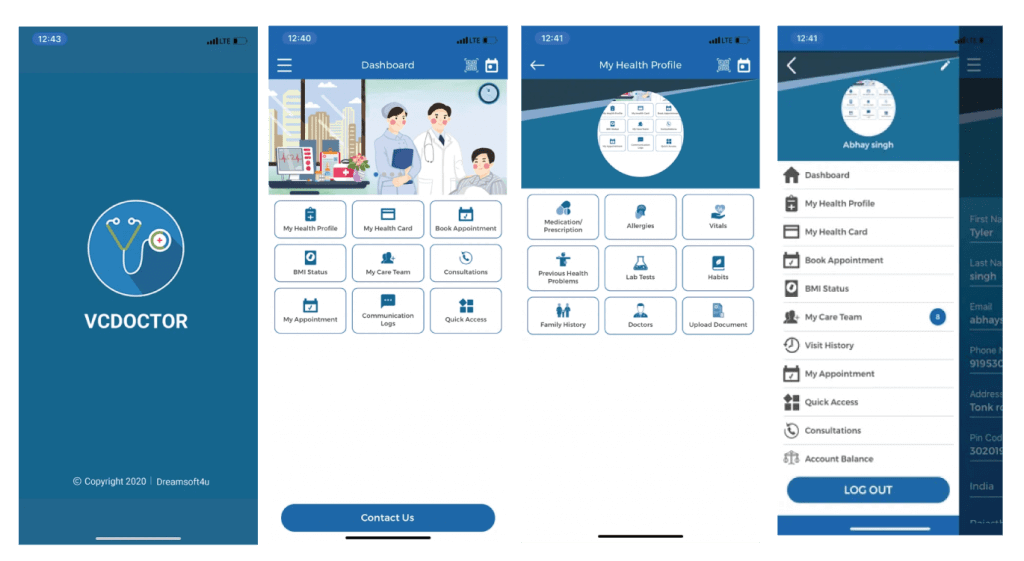
There are programs that can analyze a person’s emotional state based on their facial expressions and can be used to monitor mental well-being. Many Telehealth providers, such as VCDoctor, help other companies and patients make the most of their practice. Advances in robotic surgery allow surgeons to operate on patients from afar.
To keep pace with technological advances, Telemedicine must, of course, overcome other administrative barriers, such as restrictions on telemedicine practice under national law, national licensing requirements for medical commissions, and reimbursement policies that affect doctors and patients out-of-pocket.
If you want to get help with any software solutions related to Telemedicine, VCDoctor has a full-fledged solution for all your varying needs. Our team has qualified experts with diversified experience in the healthcare sector. We have helped several customers in fulfilling their telemedicine business and enhance their overall productivity.
FAQs
Q: What is telemedicine?
A: Telemedicine refers to the use of technology to provide medical care remotely, such as through video conferencing or online platforms.
Q: Is telemedicine safe and effective?
A: Yes, telemedicine has been proven to be safe and effective for many medical conditions. It lessens the need for in-person visits by enabling patients to get medical treatment from the convenience of their own homes.
Q: Is telemedicine only for minor health issues?
A: No, telemedicine can be used for a wide range of health issues, including both minor and major conditions. It can be used for routine check-ups, chronic disease management, mental health consultations, and more.
Q: Are telemedicine appointments as good as in-person appointments?
A: Yes, telemedicine appointments can be just as effective as in-person appointments for many medical conditions. Studies have shown that telemedicine can lead to comparable outcomes and patient satisfaction levels.
Q: Is telemedicine only for tech-savvy patients?
A: No, telemedicine is designed to be accessible to a wide range of patients, regardless of their level of technical expertise. Many telemedicine platforms are user-friendly and offer support for patients who may need assistance.
Q: Is telemedicine covered by insurance?
A: Many insurance plans cover telemedicine services, especially in light of the COVID-19 pandemic. It’s best to check with your insurance provider to confirm your coverage.
Q: Is telemedicine only for rural areas?
A: No, while telemedicine can be particularly beneficial for patients in rural or remote areas with limited access to healthcare, it can also be used by patients in urban areas. Telemedicine offers convenience and accessibility to patients regardless of their location.
Q: Is telemedicine less personal than in-person visits?
A: Telemedicine appointments can be just as personal as in-person visits, with healthcare providers able to provide personalized care and attention through video conferencing or online platforms.
Q: Is telemedicine here to stay?
A: Yes, telemedicine has gained significant traction during the COVID-19 pandemic and is expected to continue to be an integral part of healthcare delivery even after the pandemic. It offers convenience, accessibility, and flexibility for both patients and healthcare providers.
Q: Is telemedicine secure and private?
A: Yes, telemedicine platforms are designed to be secure and compliant with patient privacy regulations, such as HIPAA in the United States. Patient information is protected during telemedicine appointments to ensure privacy and confidentiality.




